ForwardHealth: The HealthCheck Benefit Helps Children and Young Adults Stay Healthy
HealthCheck is a Medicaid health care benefit for people under 21. HealthCheck can help prevent illnesses and find and treat health issues early.
The benefit covers most services and items for people under 21 who have Medicaid coverage. If they have a ForwardHealth card, they have Medicaid.
The HealthCheck benefit
There aren’t any new or additional forms for HealthCheck. HealthCheck covers the member’s well-child check, follow-up visits, and special appointments.
Well-child checks
Well-child checks are medical visits that members under 21 go to when they are not sick. The provider asks questions and examines them to make sure they’re healthy and taking the right steps to stay that way. It’s a good time for members and their caregivers to ask health questions. Well-child checks follow guidelines from the American Academy of Pediatrics’ Preventive Care Schedule. Things that happen at a well-child check include:
- Dental checks
- Growth and development checks
- Head-to-toe physical exams
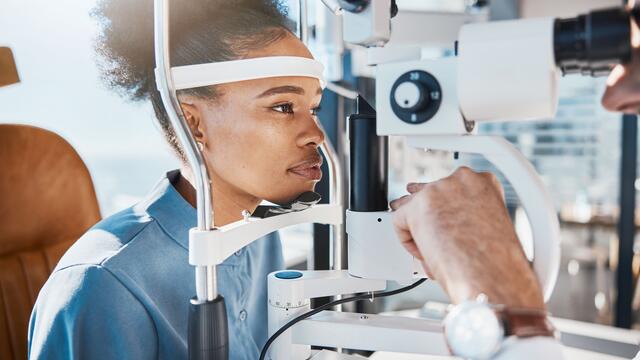
- Hearing and vision checks
- Immunizations
- Lab tests
- Nutrition checks
Follow-up visits and special appointments
The provider may find things that should be looked at further. For example:
- Dental concerns
- Ear or eye concerns
- Growth and developmental milestones
- Mental, emotional, or substance use concerns
- Needed tests or vaccines
- Other medical concerns
Any follow-up visits or special appointments that are made due to something found during a well-child check are covered by HealthCheck.


Costs
There is no cost for a well-child check. Well-child checks, follow-up visits, and special appointments are covered with the member’s ForwardHealth card.
HealthCheck Other Services
Members under 21 can use a benefit called HealthCheck Other Services to get services or items Medicaid typically doesn’t cover.
The service or item must be:
- Prescribed by the member’s provider
- Able to be covered according to federal Medicaid law
- Approved by their health plan or Wisconsin Medicaid, based on information submitted by the member’s health care provider
Some common services or items included under HealthCheck Other Services are:
- Behavioral and mental health treatment
- Durable medical equipment
- Disposable medical supplies
- Orthodontia
- Over-the-counter items
- Personal care services
Help with finding a provider and getting to a medical appointment or pharmacy
Get help finding a provider by calling ForwardHealth Member Services at 800-362-3002.
If a member needs a ride to a medical appointment or pharmacy, they can use our non-emergency medical transportation benefit. Members may be able to get a ride, bus tickets, or money for gas. Call 866-907-1493 to schedule a ride or visit our non-emergency medical transportation page for more information.
More information about HealthCheck and HealthCheck Other Services
- FAQs (frequently asked questions) about HealthCheck
- HealthCheck Brochure, P-01007 (PDF)
- HealthCheck Mini Poster, P-01007a (PDF)
- HealthCheck Other Services for Over-the-Counter Drug Coverage Member Flyer, P-03630 (PDF)
Resources for professionals
- County waiver agencies: HealthCheck: Information for County Waiver Agencies
- Providers: Resources for HealthCheck Providers
- BadgerCare Plus: Covered Services and Copays
- Immunizations: Childhood and Adolescent Vaccine Information
- Children’s Long-Term Support: Program Information for Families
- Oral Health Program: Information for All
- Lead-Safe Wisconsin: Pediatric Lead Testing and Reporting
- Maternal and Child Health: Well Badger Resource Center
