Wisconsin Coverdell Stroke Program: Stroke Systems of Care
The American Stroke Association (ASA) describes the following elements as transitions within a stroke survivor’s system of care: “from prehospital to the admitting hospital, from the intensive care unit to the hospital floor, from the hospital to post-acute settings (inpatient rehabilitation, skilled nursing facility, long-term acute care hospital, or home), and from a facility to home.”
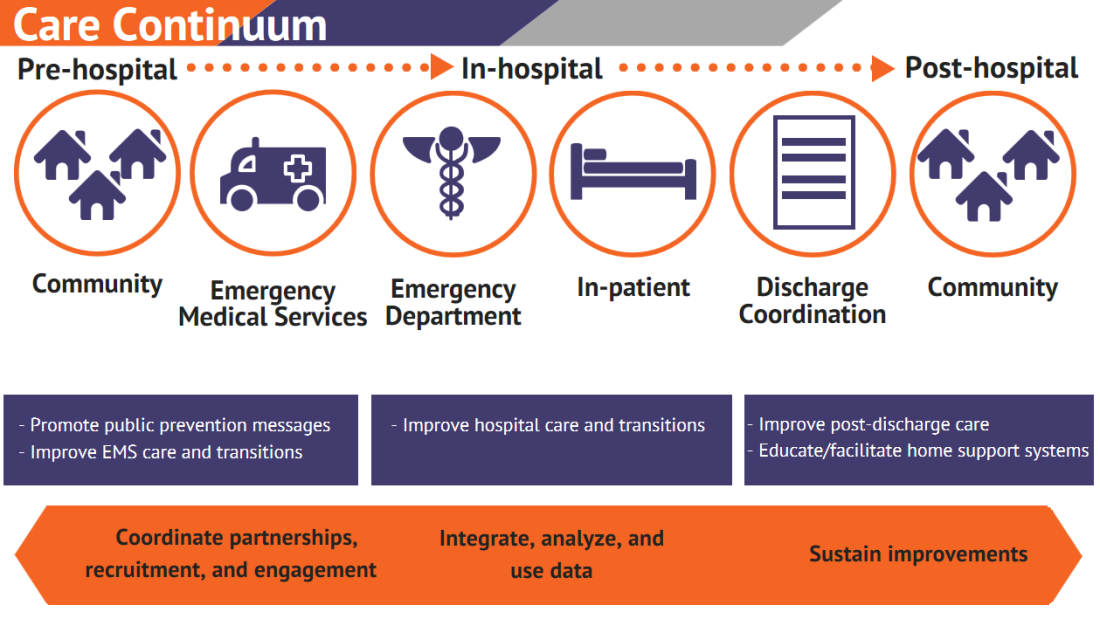
A key goal of the Wisconsin Coverdell Stroke Program is to create efficiencies in patient care transitions in Wisconsin. To reach this goal, we partner with stakeholders at the state and national levels. These partnerships with stakeholders help to create stroke systems of care guidelines and share promising practices. These efforts continue to increase the quality and efficiency of stroke care across the care continuum, as illustrated in the graphic below.
The ASA’s Recommendations for the Establishment of Stroke Systems of Care: A 2019 Update provides guidance for policymakers and public health care agencies to update their stroke systems of care. These revisions should be based on ASA’s comprehensive review of scientific evidence, evaluating current stroke care, and updates to the ASA’s previous recommendations for improvements in stroke systems of care.
Recommendations for improving Stroke Systems of Care
The following areas of focus related to improving care transitions and reducing disparities in stroke care have been identified by the ASA and the Wisconsin Coverdell Stroke Program. Researchers and providers agree that improvement and increased understanding in these areas will lead to improved patient outcomes.
- Further advance public knowledge on prevention, risk factors, and signs and symptoms of stroke.
- Encourage primary prevention with a particular focus on earliest (primordial) risk factors that can lead to stroke.
- Improve and facilitate acute therapy.
- Advance secondary prevention and recovery from stroke.
- Develop stroke programs in a coordinated and collaborative fashion, involving providers and policy makers at the local, state, and national levels.
Root causes of ineffective care transitions
In addition to providing the focus areas detailed above, the ASA has identified three primary root causes of ineffective transitions of care. Root causes often differ from one health care organization to another, but those most often described in medical literature and by experts include breakdowns in:
- Communication.
- Patient education.
- Accountability.
More details can be found in Recommendations for the Establishment of Stroke Systems of Care: A 2019 Update by the ASA.
Care continuum
The Wisconsin Coverdell Stroke Program supports comprehensive stroke systems across the continuum of care. These systems help all individuals, those at highest risk for stroke events, as well as stroke patients. The keys to any successful patient transition across the care continuum are to:
- Establish partnerships.
- Have open communication.
- Assess accountability.
Get With The Guidelines® is a stroke registry. Participating hospitals enter stroke abstracts into the registry. It captures the care continuum in various settings:
- Prehospital (special initiatives)
- In hospital
- Post discharge (discharge, mortality, and readmission)
This data infrastructure allows hospitals to take two steps. First, they can measure, track, and assess the quality of stroke care data. Second, they can begin initiatives to improve performance and ensure seamless transitions of care.
The Wisconsin Coverdell Stroke Program offers support for improving overall stroke care across the care continuum. Running data from Get With The Guidelines® assists us in measuring if we have met our goals. Coverdell provides quarterly report cards with comparative benchmarks. This allows hospitals to analyze their performance. The program also holds quarterly meetings where we analyze and discuss data across the care continuum. These meetings also allow for networking and sharing best practices.
We strongly encourage Coverdell participants to enter data across the continuum into the registry. Consider the benefits and feasibility for your organization. Entering this data allows you to assess pre-arrival, and in patient care along with post hospital discharge transitions which can lead to improved comprehensive care across the entire continuum.
Articles, guidelines, and webinars
- Taking an Accurate Blood Pressure Reading – Outpatient Adults—A guide for teaching staff how to take an accurate blood pressure reading
- Patient Self-Measurement of Blood Pressure—A guide for teaching patients how to self-monitor their blood pressure at home
- Social Determinants of Health and Stroke Series—Insight from the Wisconsin Hospital Association
Contact us
Dot Bluma, BSN, RN, CPHQ
MetaStar stroke project specialist
dbluma@metastar.com