Mpox: Basic Information
Mpox is a rare but potentially serious disease that is caused by the mpox virus. Mpox virus is from the same family of viruses as the smallpox virus. It is also less severe and transmissible than smallpox. Mpox can spread from infected humans, animals, and materials contaminated with the virus.
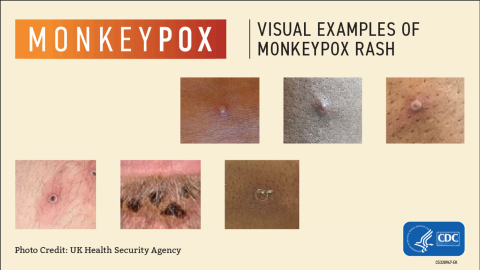
Mpox virus is characterized by a new, unexplained rash and skin lesions. It is usually found in Central and West Africa and normally does not spread in the United States. In May 2022, mpox began spreading in countries where the virus normally is not found, including in the United States. In this global outbreak, cases are linked to prolonged close, personal contact with other people who are sick.
The CDC (Centers for Disease Control and Prevention) continue to receive reports of cases that reflect ongoing community transmission in the United States and internationally. Mpox is not currently a risk for most people, however vaccination is still recommended for gay, bisexual, and other men who have sex with men.
Mpox 101
Mpox does not spread easily from person to person. People must have close, sustained contact with an infected person to get the virus. Mpox can spread through:
- Respiratory or oral secretions
- Close physical contact
- Touching sores or body fluids
- Touching personal belongings that have had contact with sores.
Mpox can also be spread to people from animals through bites, scratches, preparation of meat or use of a product from an infected animal.
Mpox is typically characterized by a new, unexplained rash that develops into hard, round, fluid or pus-filled skin lesions. Other early symptoms include:
- Fever
- Swollen lymph nodes
- Muscle aches
- Chills
The mpox rash usually develops within one to three days after fever. However, some people may experience a rash or sores first, followed by other symptoms.
Some people may also only develop a rash.
If you have mpox symptoms, talk with a healthcare provider, ask about getting tested for mpox, isolate at home, and avoid close physical contact until a health care provider can examine you.
Most people who have mpox recover without needing treatment within two to four weeks. While there is no specific treatment for mpox, antiviral medications that have been used to treat smallpox can be used.
People who have been exposed to someone with mpox are eligible to receive a vaccine to prevent the onset of disease or reduce the severity of symptoms. DHS will work with healthcare providers to obtain vaccines and treatment when necessary.
Vaccination helps protect against mpox when given before or shortly after an exposure.
Most people with mpox report having prolonged close contact with someone with mpox. The mpox virus is unlikely to linger in the air or spread through the air over long distances. To protect yourself from mpox, take the following actions:
- A safe and effective vaccine is available for certain people who have a higher risk of getting sick.
- Avoid skin-to-skin contact, including sex and intimate contact, with someone who has a rash or other symptoms.
- Ask your sexual partner(s) if they have a rash or other mpox related symptoms.
- Consider how much close, skin-to-skin contact is likely to occur at the event you plan to attend.
- Do not share objects like bedding, towels, clothing, or utensils with someone with mpox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
- If you are in Central or West Africa, avoid contact with animals that can spread mpox virus, usually rodents and primates.
If you were exposed to mpox, monitor for symptoms for 21 days after your date of last exposure. It is important to check your temperature two times per day during your monitoring period.
- Mpox Virus, P-03284 (PDF)
- Mpox Symptom Monitoring, P-03287 (PDF)
- Mpox | Poxvirus | CDC
- How to Protect Yourself | Mpox | Poxvirus | CDC
- Safer Sex, Social Gatherings, and Mpox | Mpox | Poxvirus | CDC
- Vaccines | Mpox | Poxvirus | CDC
- Mpox Infections after Vaccination | Mpox | Poxvirus | CDC
- State of Vaccine Confidence Insights Report: Mpox in Chicago Special Report | CDC (PDF)
- 'Greater Than' Digital Graphics and Outreach Materials | Kaiser Family Foundation
- Mpox Communications Toolkit | National Coalition of STD Directors
Questions about mpox? Contact us! Phone: 608-267-9003 | Fax: 608-261-4976
Wisconsin Local Health Departments – Regional offices – Tribal agencies