Immunizations: Meningococcal Vaccines
Meningococcal disease refers to any illness caused by the meningococcal bacterium (also called Neisseria meningitidis).
These illnesses often are severe and can be deadly.
The bacteria infect the blood, brain, and spinal cord. This is one of the most common causes of bacterial meningitis.
Vaccines can prevent meningococcal disease
The best way to prevent meningococcal disease is to stay up to date with recommended vaccines.
Learn more about vaccines for meningococcal disease
Meningococcal disease 101
About 1 out of 10 people carry meningococcal bacteria in their nose and throat, but don't get sick. These people are known as carriers. Although carriers don’t have any signs or symptoms, they still can spread the bacteria and make others sick.
Meningococcal bacteria spread from person to person through saliva or spit, for example, when coughing or kissing. The bacteria can spread to people who’ve had close or lengthy contact with someone who has meningococcal disease. Close contact also includes sharing items that come in contact with the mouth (water bottles, eating utensils, lip balm, cigarettes and smoking materials).
People don’t catch the bacteria through casual contact or by breathing air where someone with meningococcal disease has been. Sometimes the bacteria can spread to people who spend a long time in the same space together, such as roommates.
Anyone can get meningococcal disease, but some people are at higher risk.
- Infants, preteens, teens, and young adults have the highest rates of meningococcal invasive disease in the United States.
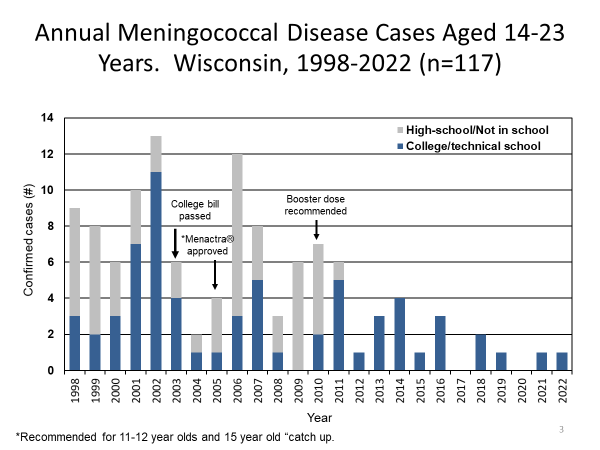
- College students and military recruits also have slightly higher risk for the disease because they spend more time in crowded living spaces, like dorms or barracks.
- People have certain medical conditions as a risk factor, like having a damaged or removed spleen.
- See Risk Factors for Meningococcal Disease.
Meningococcal disease is very serious and can be deadly in a matter of hours. It’s important to get medical attention right away if you have the symptoms listed below.
Unfortunately, meningococcal disease can be hard to diagnose. The signs and symptoms are often similar to those of other illnesses. That’s why it’s important to get vaccinated before it’s too late.
Symptoms of meningococcal disease often start as flu-like illness and quickly get worse. The specific symptoms vary depending on the type of illness.
The two most common types of meningococcal infections are meningitis and septicemia.
When meningitis is caused by the bacteria Neisseria meningitidis, it’s called meningococcal meningitis. The bacteria infect the lining of the brain and spinal cord and cause swelling.
The most common symptoms include:
- Fever
- Headache
- Stiff neck
Often, there are other symptoms, such as:
- Nausea
- Vomiting
- Photophobia (eyes being more sensitive to light)
- Altered mental status (confusion)
Newborns and babies might not have these classic symptoms. Instead, babies may be slow or inactive, irritable, vomiting, feeding poorly, or have a bulging anterior fontanelle (the soft spot of the skull). In young children, doctors also may look at the child’s reflexes for signs of meningitis.
Meningococcal septicemia (or meningococcemia)
When septicemia (a blood stream infection) is caused by the bacteria Neisseria meningitidis, it’s called meningococcal septicemia. The bacteria enter the blood stream and damage the blood vessels. This causes bleeding into the skin and organs.
Symptoms may include:
- Fever and chills
- Fatigue (feeling tired)
- Vomiting
- Cold hands and feet
- Severe aches or pain in the muscles, joints, chest, or abdomen (belly)
- Rapid breathing
- Diarrhea
- In the later stages, a dark purple rash
Doctors treat meningococcal disease with antibiotics. It is important that treatment start as soon as possible. Antibiotics help reduce the risk of dying.
Depending on how serious the infection is, people with meningococcal disease may need other treatments, including:
- Breathing support
- Medications to treat low blood pressure
- Surgery to remove dead tissue
- Wound care for parts of the body with damaged skin
Even with treatment, 10 to 15 out of every 100 people with meningococcal disease will die. Up to 1 in every 5 survivors will have long-term disabilities. These may include brain damage, deafness, loss of limbs, or nervous system problems.
Staying up to date with recommended vaccines is the best protection against meningococcal disease. The CDC (Centers for Disease Control and Prevention) recommends meningococcal vaccines for all preteens and teens. In certain situations, other children and adults should get meningococcal vaccines.
Three serogroups, or types, of Neisseria meningitidis cause most meningococcal illness in the United States. These types are B, C, and Y. Other common types found around the world are A, W, and X. Vaccines can prevent almost all types of meningococcal disease.
There are two types of meningococcal vaccines:
- The MenACWY vaccine prevents infection with meningococcal types A, C, W, and Y.
- The CDC recommends MenACWY for:
- All preteens at 11–12 years old.
- Booster shot for all teens at 16 years old.
- This vaccine also is called MCV4.
- The CDC recommends MenACWY for:
- The MenB vaccine prevents infection with meningococcal type B.
- The CDC recommends a MenB vaccine for people ages 16–23 years old, especially those at high risk of meningococcal disease.
- Multiple doses of MenB are needed for the best protection. Brand names for the MenB vaccine differ by manufacturer. All doses need to be from the same brand of vaccine.
Younger children and adults usually don’t need meningococcal vaccines. However, the CDC recommends one or both types of meningococcal vaccines for people with:
- Certain medical conditions.
- Travel plans to areas where the disease is common.
- Crowded living situations like college dorms or military barracks.
- Jobs working with the bacteria.
- Increased risk due to a meningococcal disease outbreak.
Find out if you and your children are protected against meningococcal disease. Check our Wisconsin Department of Health Services (DHS) Wisconsin Immunization Registry to see if you have received vaccines labeled as “Meningo” or “Meningo B." Depending on the brand of vaccine first received, you’ll need either two or three doses to be fully protected.
Call your doctor’s office or local health department for help if you:
- Can’t find a record for yourself.
- Can’t find a record for a child in your care.
- Aren’t sure if you are up to date on your vaccines.
To find a location where you can get a vaccine, call your doctor, pharmacy, or local health department. Learn more about finding and paying for childhood, adolescent, and adult vaccinations.
If you’re worried about cost, your family may be eligible for free vaccines. Read about our Vaccines For Children and Vaccines For Adults programs.
Close contacts of a person with meningococcal disease should receive antibiotics to prevent them from getting sick. Examples of close contacts include:
- People in the same household
- Roommates
- Anyone in direct contact with a patient’s oral secretions (saliva or spit), such as a kissing partner
If you or someone you know has meningococcal disease, contact a doctor or local health department. They can help recommend who should get preventative antibiotics.
- CDC disease overview—Meningococcal Disease
- DHS disease overview—Meningococcal Disease
- CDC vaccine information statement—Meningococcal ACWY
- CDC vaccine information statement—Meningococcal B
- Immunization Action Coalition—Meningococcal Vaccine Recommendations by Age and Risk Factor for Serogroups A, C, W, or Y (PDF)
- Immunization Action Coalition—Meningococcal Vaccine Recommendations by Age and Risk Factor for Serogroup B (PDF)
- CDC—Vaccine safety
Data and statistics
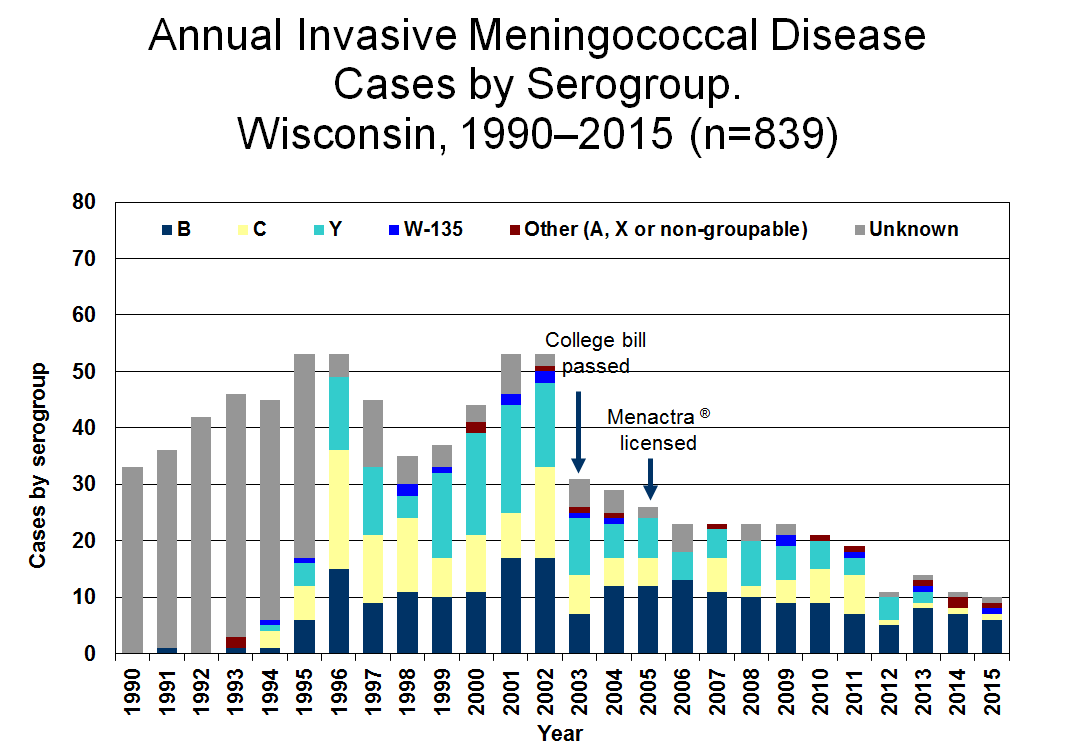
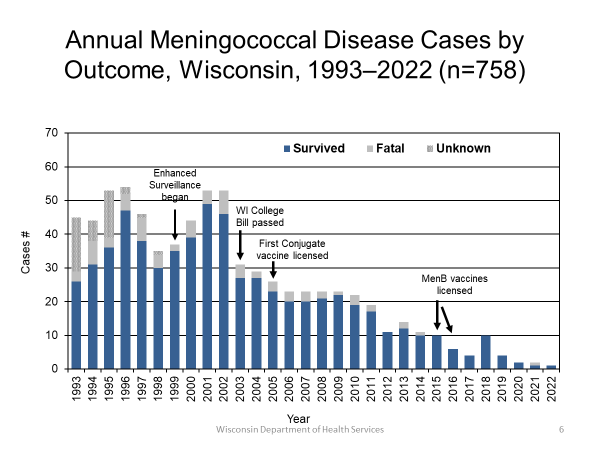
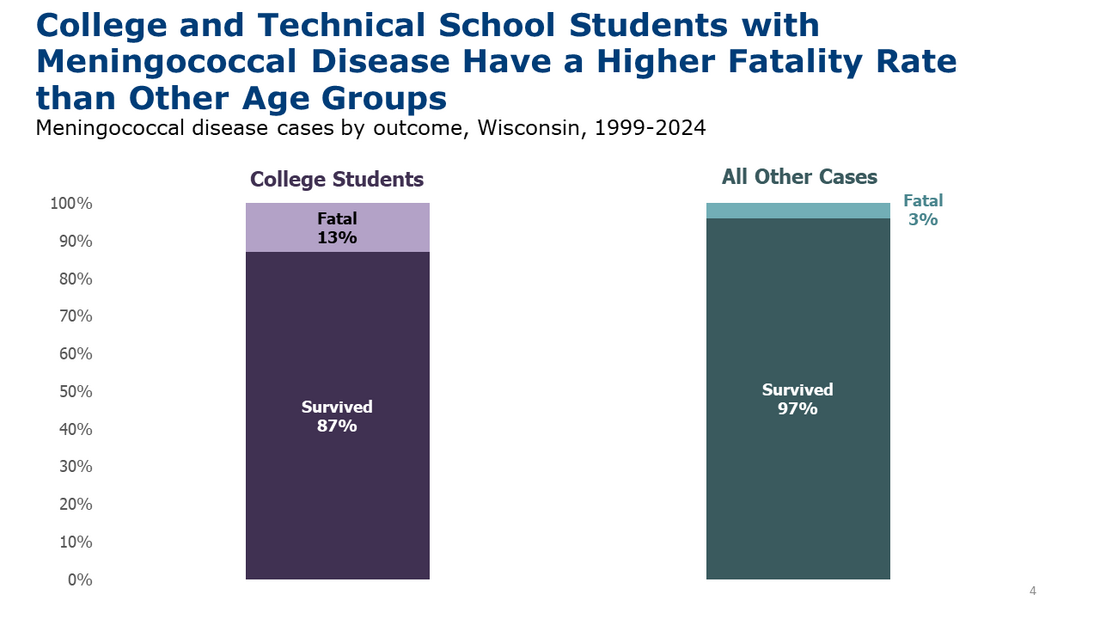
These graphs show both historical and current meningococcal disease data.
Just for health care providers
Meningococcal disease is communicable. Health care providers must report all cases of meningococcal disease.
Meningococcal disease is a Wisconsin Disease Surveillance Category I disease
Report it right away to the patient’s local public health department. Call as soon as you identify a confirmed or suspected case. The health department then notifies the state epidemiologist.
Within 24 hours, submit a case report through one of the following:
- Wisconsin Electronic Disease Surveillance System (WEDSS)
- Mail or fax—Acute and Communicable Disease Case Report, F44151 (Word)
Read more about required disease reporting in Wisconsin.
Case reporting and public health guidelines
- Case Reporting and Investigation Protocol (previously called EpiNet)—Meningococcal disease (Neisseria meningitidis), P-01975 (PDF)
- CDC recommendation from the Advisory Committee on Immunization Practices (ACIP) on meningococcal vaccines—Meningococcal ACIP Vaccine Recommendations
- Wisconsin State Library of Hygiene—Clinical Testing Reference Manual
- DHS Division of Public Health—Invasive Meningococcal Disease Protocol, P-01626 (PDF)
- DHS Division of Public Health—Meningococcal Disease Case Investigation Flowchart