STD: Antibiotic-Resistant Gonorrhea
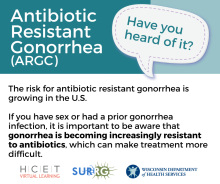
What is antibiotic-resistant gonorrhea?
Antibiotic-resistance, or antimicrobial resistance, happens when germs like bacteria develop the ability to resist, and even defeat, the drugs designed to kill them. That means the bacteria are not killed and continue to grow, and the person infected may stay sick or get sicker.
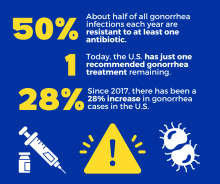
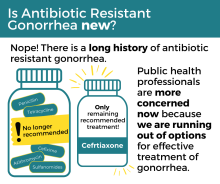
From the 1930s to today, Neisseria gonorrhoeae, the bacteria that cause gonorrhea infections, have grown resistant to nearly every drug used to treat gonorrhea. These instances are referred to as antibiotic-resistant gonorrhea
Today, the U.S. has just one recommended gonorrhea treatment option remaining: ceftriaxone. The CDC (Centers for Disease Control and Prevention) treatment guidelines (PDF) recommend:
- A single intramuscular 500mg dose of ceftriaxone for people who weigh less than 331 lbs; (150 kg).
- A single intramuscular 1000mg dose of ceftriaxone for people who weigh 331 lbs (150 kg) or more.
People with allergies to cephalosporins may be treated with a CDC-approved alternative regimen.
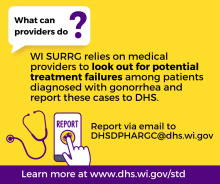
Providers and case investigators should assess for suspected treatment failure (STF) among their patients and use tests of cure (TOCs) to assess for persistent cases that may be resistant to treatment.
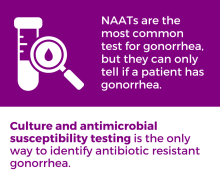
How to identify antibiotic-resistant gonorrhea
Look out for suspected treatment failure
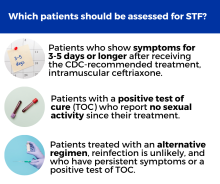
Health professionals and local and tribal health departments are advised to look out for instances of suspected treatment failure among patients treated for uncomplicated gonorrhea. Suspected treatment failure refers to cases of gonorrhea that don’t go away despite treatment with the recommended antibiotic regimen. STF should be assessed for patients whose symptoms do not resolve within three or more days after the recommended treatment and either:
- Report no sexual contact during the post-treatment follow-up period, or
- Have a positive culture on TOCs regardless of sexual activity.
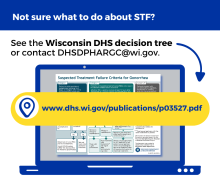
Learn how to identify suspected treatment failure, P-03527 (PDF)
Do a test of cure to be sure the infection was treated successfully
A test of cure (TOC) is follow-up testing to be sure the infection was treated successfully. This should be performed for any patients with gonorrhea isolates with reduced susceptibility, patients exhibiting signs of STF, patients with anogenital gonorrhea not treated with the recommended CDC regimen or CDC-recommended alternative regimens, and any patient with pharyngeal gonorrhea. Contact the DHS Sexually Transmitted Infections (STI) Unit antibiotic resistant gonorrhea team at DHSDPHARGC@dhs.wisconsin.gov.
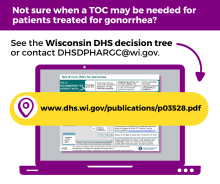
Learn more about how and when to do a TOC, P-03528 (PDF)
Order an antibiotic susceptibility test to see if the bacteria have resistance to recommended antibiotics
Antibiotic susceptibility testing is done to confirm if a patient has a type of gonorrhea that has reduced susceptibility or resistance to treatment with recommended antibiotics. A patient's sample is put on a petri dish that also contains different antibiotics used to kill the bacteria. If bacteria are able to be grown on the plate even with certain antibiotics present, that is a sign of reduced susceptibility or resistance to antibiotics. Doctors should then prescribe an alternative antibiotic regimen. See the full CDC STI Treatment Guidelines (PDF) for more information.
What is Wisconsin Department of Health Services (DHS) doing?
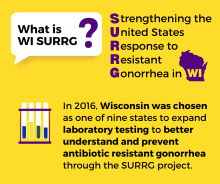
Collaborating to address antibiotic resistant gonorrhea
Since 2016, DHS has worked closely with the Milwaukee Health Department and Laboratory (MHD and MHDL) to pilot and identify best practices for responding to cases of antibiotic-resistant gonorrhea. This work was initially supported by the Strengthening the United States Response to Resistant Gonorrhea (SURRG) grant through the CDC. In 2024, DHS was awarded with the new iteration of this grant, Combatting Antimicrobial Resistant Gonorrhea and Other STIs (CARGOS).
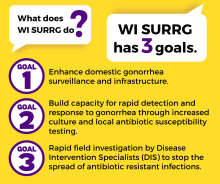
This work supports three core national goals:
- Enhance domestic gonorrhea surveillance and infrastructure
- Build capacity for rapid detection and response to antibiotic-resistant gonorrhea through increased culturing and local antibiotic susceptibility testing
- Rapid field investigation to stop the spread of resistant infections
Collaboration with and effort by clinical, laboratory, and data staff is crucial to advance these goals and address antibiotic-resistant gonorrhea.
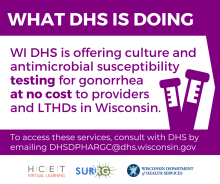
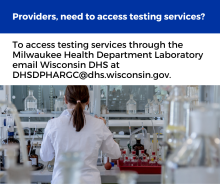
Expanding capacity for antibiotic-resistant gonorrhea testing
Each state participating in SURRG has worked to implement a Center of Excellence (COE) within their home state. COEs serve as hubs for enhanced antibiotic-resistant gonorrhea testing services and the identification of best practices for antibiotic-resistant gonorrhea diagnostics. The Milwaukee Health Department Laboratory is the statewide COE for Wisconsin. This means DHS and CDC funds them to assist health care providers and public health practitioners to access antibiotic-resistant gonorrhea testing at no cost.
Health care providers or public health providers across Wisconsin can access no-cost diagnostic services for antibiotic-resistant gonorrhea, including:
- Culture of samples.
- TOC.
- Antibiotic susceptibility testing.
- Consultation for alternative treatment decisions.
If you or your clinic would like to request these services or have questions, contact the DHS Sexually Transmitted Infections (STI) Unit antibiotic resistant gonorrhea team at DHSDPHARGC@dhs.wisconsin.gov.
Resources for health professionals and local and Tribal health departments in Wisconsin
- Cephalosporin-Resistant Outbreak Response Plan
- DHS decision making resources
- DHS medical guidance
- Nguyen TQ, Jamison K, Pfister J, Sankaran M, Amsterdam L, Siemetzk-Kapoor U, Pathela P. Targeting Culture Criteria to Maximize Culture Positivity of Neisseria gonorrhoeae in 3 Sexual Health Clinic Settings. Sex Transm Dis. 2021 Dec 1;48(12S Suppl 2):S144-S150. doi: 10.1097/OLQ.0000000000001528. PMID: 34407013.
- Health Alert: Current Drug Shortages Affecting Treatment of Syphilis and Gonorrhea
- Clinical and Laboratory Guidance for Suspected Treatment Failure Among Patients Treated (PDF)
- CDC guidelines and resources
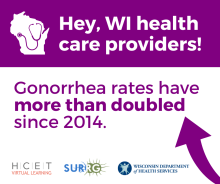
Social media posts
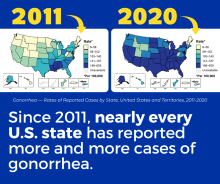
Caption: Are you a health care provider in Wisconsin? Given the rise in gonorrhea and increased risk for antibiotic resistance over the past decade, it is important to order the right test for your patient. Only culture tests and antibiotic susceptibility tests (AST) can identify resistance. Wisconsin DHS offers these tests at no cost for eligible providers and local and Tribal health departments. Contact dhsdphargc@dhs.wisconsin.gov to learn more.
Caption: As Wisconsin works to better understand and prevent antibiotic resistant gonorrhea, health care providers and other people in Wisconsin can help too. From 2016-2024, Wisconsin's antibiotic resistant gonorrhea work was funded through the CDC's SURRG grant. As of 8/1/2024, SURRG has transitioned to the Combating Antibiotic Resistant Gonorrhea and Other STIs (CARGOS) grant. CARGOS will continue to fund Wisconsin's antibiotic resistant gonorrhea work through at least 2029. Learn more at www.dhs.wisconsin.gov/std/argc.htm.
Learn how to practice and advocate for safer sex and regular testing for sexually transmitted infections (STIs). To be better prepared, look out for symptoms that don't go away after treatment for gonorrhea.
Caption: As a health care provider, you know that gonorrhea treatment is becoming more complicated because of antibiotic resistance. If a patient's condition isn't responding to the CDC-recommended treatment, it could be a sign of antibiotic resistance. Learn more at www.dhs.wisconsin.gov/std/argc.htm.
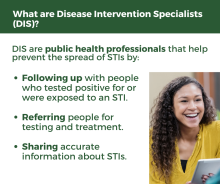
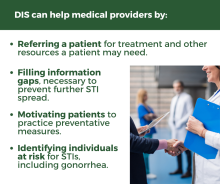
Caption: STI prevention work is an important part of keeping Wisconsinites healthy and wouldn’t be possible without dedicated Disease Intervention Specialists (DIS), who help people access testing and treatment services for themselves and their partners. We thank our DIS for their hard work and encourage everyone to learn more about their role in keeping Wisconsinites safe and healthy! Learn more at www.dhs.wisconsin.gov/std/argc.htm #TalkTestTreatRepeat
Caption: Are you a health care provider in Wisconsin? Given the rise in gonorrhea rates/cases? and increased risk for antibiotic resistance over the past decade, it is important to make sure treatment is effective. This may be done with test of cure, appropriate for most patients 14 days or more following treatment. If the test comes back positive or you have reason to suspect a resistant case of gonorrhea, the Department of Health Services can help you access diagnostic services. Contact dhsdphargc@dhs.wisconsin.gov to learn more.
Caption: Gonorrhea treatment can be a little complicated. If you have recently been treated for gonorrhea, you can make sure that the infection has been cleared by getting a follow up test from your provider. Learn more at www.dhs.wisconsin.gov/std/argc.htm.
Caption: Are you a health care provider in Wisconsin? It’s important to make sure that treatment was effective for your patients. If a patient is infected with a strain of gonorrhea resistant to recommended antibiotics, they may present as a case of suspected treatment failure (STF) and need additional testing. These services are accessible through the Department of Health Services for eligible patients at no cost to the clinic or LTHD. Contact dhsdphargc@dhs.wisconsin.gov to learn more.