Legionellosis (Legionnaires' Disease and Pontiac Fever)
Legionellosis in an infection caused by Legionella bacteria.
There are two different types of legionellosis:
- Pontiac fever
- Legionnaires' disease
Pontiac fever is a mild respiratory illness and Legionnaires' disease is more severe and is a type of pneumonia.
Legionnaires' disease is not normally spread from person to person.
Are you a health care provider? Find information on testing, reporting, surveillance, and prevention.
Legionellosis 101
Legionella bacteria are found naturally in freshwater and moist environments (for example, lakes, rivers, groundwater) worldwide. Legionella can become a public health problem in manmade water systems, where it can grow and spread, causing disease. Most healthy people who are exposed to Legionella do not become sick. However, people aged 50 years or older, smokers, and those with underlying medical conditions such as chronic lung disease, or those with a weakened immune system, are at higher risk of becoming sick from Legionella or with legionellosis.
Outbreaks of Legionnaires’ disease are most commonly associated with large or complex water systems (e.g., hospitals, long-term care facilities, hotels, cruise ships).
People can become sick when they breathe in mist from a water source that has Legionella (water used for showering, cooling towers, decorative fountains, and hot tubs). This CDC (Centers for Disease Control and Prevention) infographic (PDF) helps illustrate how Legionella is spread.
Common signs and symptoms of legionellosis are:
- Muscle aches
- Headache
- Tiredness
- Loss of appetite
- Coughing
- Fever
- Diarrhea (occasionally)
Contact your doctor if you develop symptoms, such as fever, cough, chills, or muscle aches. Be sure to mention if you spent any nights away from home in the last 10 days.
Treatment depends on whether or not the person has Pontiac fever or Legionnaires' disease. Pontiac fever requires supportive care only and will go away on its own. Legionnaires' disease is treated with antibiotics.
Most people who get sick need care in a hospital but make a full recovery. However, about 1 out of 10 people who get Legionnaires’ disease die from the infection.
There are no vaccines against Legionella bacteria.
To prevent Legionella bacteria from growing, it is important to make sure that water systems in buildings are being properly cared for and maintained.
CDC web resources on Legionella prevention
Legionnaires’ disease is on the rise in Wisconsin and nationally. The rising trend may be related to a combination of factors, such as increased awareness and testing, more people at risk (e.g., aging population, use of immune-suppressing medication), and increased Legionella in the environment.
Because Legionnaires’ disease is likely underdiagnosed, the number of cases may be underestimated. More illness is usually found in the summer and early fall, but it can happen any time of year.
- Legionellosis Fact Sheet, P-42066 (Multiple Languages): Educational fact sheet for the general public on legionellosis covering signs and symptoms, treatment, and prevention
- About Legionellosis: CDC webpage including information on symptoms, diagnosis, possible causes of legionellosis, treatment, and prevention
- Legionellosis resources: CDC webpage containing resources for patients and their families
- How Legionella affects building water systems and people: CDC infographic illustrating how Legionella is spread
Just for health care providers
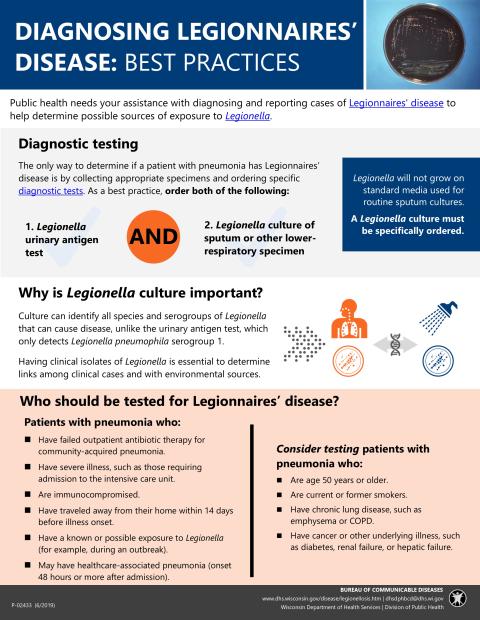
We request assistance from health care providers, laboratorians, and local and tribal public health agencies with diagnosing, P-02433 (PDF) and reporting, P-1895 (PDF) cases of Legionnaires' disease to help promptly determine possible sources of exposure to Legionella so that we may prevent further infections. See detailed information below.
Legionnaires' disease is a Wisconsin Disease Surveillance Category II Disease
- Report to the patient's local public health department electronically, through the Wisconsin Electronic Disease Surveillance System (WEDSS), by mail or fax using an Acute and Communicable Disease case report, F-44151 (Word) or by other means within 72 hours upon recognition of a case.
- Information on communicable disease reporting
Case reporting and public health follow-up guidelines
Case Reporting and Investigation Protocol (previously called EpiNet): Legionellosis, P-01895 (PDF)
Testing
Testing for Legionnaires’ disease is recommended for patients with pneumonia who:
- Have failed outpatient antibiotic therapy for community-acquired pneumonia
- Have severe illness, such as those requiring admission to the intensive care unit
- Are immunocompromised
- Have traveled away from their home within 14 days before illness onset
- Have a known or possible exposure to Legionella (for example, during an outbreak)
- May have healthcare-associated pneumonia (onset 48 hours or more after admission)
The urinary antigen assay and culture of lower respiratory secretions on selective media (buffered charcoal yeast extract [BCYE] agar) are the preferred diagnostic tests, P-02433 (PDF) for Legionnaires’ disease.
We strongly encourage clinicians to order both Legionella cultures and urinary antigen tests for any patients suspected of having Legionnaires’ disease.
Of note, culturing lower respiratory specimens (e.g., sputum or bronchoalveolar lavage) from patients infected with Legionella may allow for the detection of all species and serogroups of Legionella, unlike the urinary antigen test, which detects only Legionella pneumophila serogroup 1 (responsible for 80 percent of Legionnaires' disease).
Please note: Legionella will not grow on standard media used for routine respiratory cultures. Thus, Legionella culture must be specifically ordered to allow for isolate recovery. Characterization of clinical isolates of Legionella is essential to determine linkages between clinical cases and environmental sources.
If your laboratory does not perform Legionella culture, specimens should immediately be sent to a reference lab such as the Wisconsin State Laboratory of Hygiene (WSLH) for testing. DPH will approve fee-exempt testing for Legionella (PCR and culture of lower respiratory specimens, pleural fluid, lung tissue, or other normally sterile site) at the WSLH for patients meeting the criteria above who have clinical or radiographic evidence of pneumonia.
To obtain approval for fee-exempt testing of these specimens, please contact the DPH Bureau of Communicable Diseases at 608-267-9003.
Additional resources
If your laboratory does not perform Legionella culture, DPH will approve fee-exempt testing for Legionella (PCR and culture of lower respiratory specimens, pleural fluid, lung tissue, or other normally sterile site) at the WSLH for patients who have clinical or radiographic evidence of pneumonia or for patients with pneumonia who:
- Have failed outpatient antibiotic therapy for community-acquired pneumonia
- Have severe illness, such as those requiring admission to the intensive care unit
- Are immunocompromised
- Have traveled away from their home within 14 days before illness onset
- Have a known or possible exposure to Legionella (for example, during an outbreak)
- May have healthcare-associated pneumonia (onset 48 hours or more after admission)
To receive approval for fee-exempt testing of these specimens, contact the DPH Bureau of Communicable Diseases at 608-267-9003.
Important note: For patients with a positive Legionella urine antigen test result, please send residual sputum or other lower respiratory specimens to the WSLH for fee exempt Legionella PCR and culture as part of our enhanced surveillance efforts. DHS approval for testing is not required for patients with positive urine antigen tests.
Laboratories sometimes reject lower respiratory specimens during a work-up for pneumonia based on specimen quality (e.g., due to lack of white blood cells/polymorphonuclear leukocytes in the sample or contamination with other bacteria). However, laboratories should not reject lower respiratory specimens for these reasons when testing for Legionnaires’ disease because Legionella can often be recovered on selective media (BCYE agar plus antibiotics which inhibit normal respiratory tract flora), and sputum produced by patients with Legionnaires’ disease may not have many white blood cells (see the CDC-recommended Specimen Collection section).
Important note: Forward all clinical Legionella isolates or lower respiratory specimens that are positive for Legionella on PCR to the WSLH for further characterization using pulsed field gel electrophoresis or whole genome sequencing. Specimens should be shipped to:
Wisconsin State Lab of Hygiene Attn: Bacteriology
2601 Agriculture Drive, Madison, WI 53718.
If needed, specimens may be shipped fee-exempt to WSLH by contacting Gold Cross Courier Service at 800-990-9668 to arrange package pick-up. If you have questions regarding specimen kits and shipping, please contact the WSLH Customer Service at 800-862-1013.
Additional resources
Investigations of clusters of Legionnaires’ disease, P-01895 (PDF) depend on aggressive follow-up of the case-patients’ history and possible exposures to Legionella. The case-patient or a member of their family should be interviewed to determine possible sources of their illness as soon as possible following diagnosis.
After the patient interview, please enter data into the Wisconsin Electronic Disease Surveillance System (WEDSS), completing all exposure fields. A webinar training is available for local and Tribal health department (LTHD) case investigators on the WEDSS SharePoint site.
Important note: If the case-patient reports staying in a lodging, health, or long-term care facility during the 14 days prior to illness onset, please notify the state legionellosis surveillance coordinator, Frances Goglio, by email at Frances.Goglio@dhs.wisconsin.gov or phone 608-267-9003 as soon as possible.
Additional resources
Environmental prevention measures
Legionnaires' disease can be prevented by minimizing growth in building water systems. This is accomplished with development and implementation of a comprehensive water management program complaint with American Society of Heating, Refrigerating, and Air Conditioning Engineers (ASHRAE) Standard 188. Centers for Medicare & Medicaid Services requires hospitals, and long-term care facilities (PDF) to implement a water management program meeting this industry standard. The CDC (Centers for Disease Control and Prevention) developed a toolkit to assist with developing a water management program. Developing a water management program is also recommended in some other settings. Use this CDC checklist to assess the needs for a water management program.
Additional resources
Toolkits, trainings, and templates
- Buildings at Risk for Legionella (CDC)
- Legionella Control Toolkit (CDC)
- Preventing Legionnaires’ Disease: A Training on Legionella Water Management Programs (PreventLD Training) (CDC)
- CDC Toolkit: Prevention of Legionnaires’ disease with Water Management Programs (CDC)
- CSTE Water Management Program Evaluation Tool and Excel Supplement
- Water Management Program Template (CSTE)
- CMS Surveyor Training Webinar: Legionella and Other Water Pathogens (CMS)
- Legionella and other Water Management Issues in Long-Term Care Facilities Webinar (PowerPoint Slides)
Fact sheets and FAQs
- Fact sheet: Growth and spread of Legionella (CDC)
- Fact sheet: Legionella water management programs (CDC)
- FAQs: Healthcare Water Management Programs (CDC)
Special considerations
- Considerations When Working with Legionella Consultants (CDC)
- Fact sheet: Hot Water Temperatures in Adult Family (DHS), P-01942 (PDF)
- Forms and Checklists: Construction and Remodeling for Health Care Facilities (DHS)
- Plumbing Plan Review in Health Care Facilities in Wisconsin (PDF) (Wisconsin Department of Safety and Professional Services)
Questions about Legionnaires’ disease can be directed to Frances Goglio, Legionellosis Surveillance Coordinator, by email Frances.Goglio@dhs.wisconsin.gov or phone 608-266-2568. Questions about environmental Legionella can be directed to Bruce Meiners, Legionella Industrial Hygienist, by email at Brucee.Meiners@dhs.wisconsin.gov or phone 608-267-1887.